In the self-insured world, “centers of excellence” is a termthat is beginning to be used for a specific hospital that has beenselected by a large employer for bundled pricing of high-ticket,higher-volume surgeries like knee replacement. The label aloneheightens expectations of vastly superior health care. Consumerswant to believe they will experience care that is off the charts inall respects; from advanced techniques, expedited treatment andlength of stay, pain management and overall patient satisfaction.The name implies that centers of excellence (COEs) are somewhatimmune to the inherent dangers of hospitalization. This expectationpersists, despite a recent study estimating that a quarter of a milliondeaths are caused by medical errors each year.
|The assumption most employees have about COEs is that they arefirst and foremost selected based on performance; that objectivemeasures of outcomes like mortality and complications are topselection criteria. They expect that only after the performancequality is determined are prices taken into consideration to findthe best value. They assume that centers of excellence live at theintersection of amazing quality and good price.
|Rise in popularity
With the rapid increase in cost of health care over the lastdecade, self-insured employers have sought outlower cost structures by engaging directly with hospitals. This trend is a big part of what is driving the popularity ofCOEs. These are typically hospitals with great name recognitionthat contract directly with self-insured employers to providefantastic deals for paying cash or expedited payment terms. Thehospital is happy because they improve their cash flow (bypassinginsurance companies whose payments are often delayed by months),employers are happy because they are often paying less money, andthe employees are happy because they believe they are going to aplace that has been vetted as “the best of the best.” On thesurface, it seems everybody wins.
|Lack of outcomes transparency
Unfortunately, trustworthy outcomes-based metrics have not beenwidely available until recently, so as a proxy for excellence,employers have had no alternative but to identify top providersbased on name recognition and reputation.
|With this in mind, our analytics team set out to investigatewhether Centers of Excellence truly provide exceptional care. Wetackled this problem by analyzing the outcome metrics for existingCOEs. While most of these centers have great national reputations,the data show surprising areas of mediocre and even poorperformance. This included high variance in hospital outcomes across the differentprocedures performed; for example, a hospital can be exceptional athip replacement, but nowhere near as good for heart bypasssurgery.
|We would not go as far as to say there is no correlation betweenreputation and outcomes, but more often than not, one does notguarantee the other. We also found surprisingly little evidencesupporting the assumption that outcomes are the top driver of COEselection. In fact, it would appear that the top factors that driveselection are price and reputation. In other words, centers ofexcellence are always “excellent” in pricing, but not necessarily“excellent” at performance.
|The cost of poor quality
So should self-insured employers care about quality? Why upsetthe apple cart if no one is complaining?
|If a quarter of a million deaths from medical errors isn’tenough of a reason to care about quality, how about the fact thatpoor health care quality costs payers hundreds ofbillions of dollars a year?
|A series of studies conducted recently by MPA HealthcareSolutions in Chicago showed that poor performing providers pose twotimes greater risk of adverse outcomes (such as severecomplications or mortality) in colon and cardiac surgery, and three times greater risk of adverseoutcomes in gall bladder surgery, hip, knee, kidney removal, and lungresection surgery.
|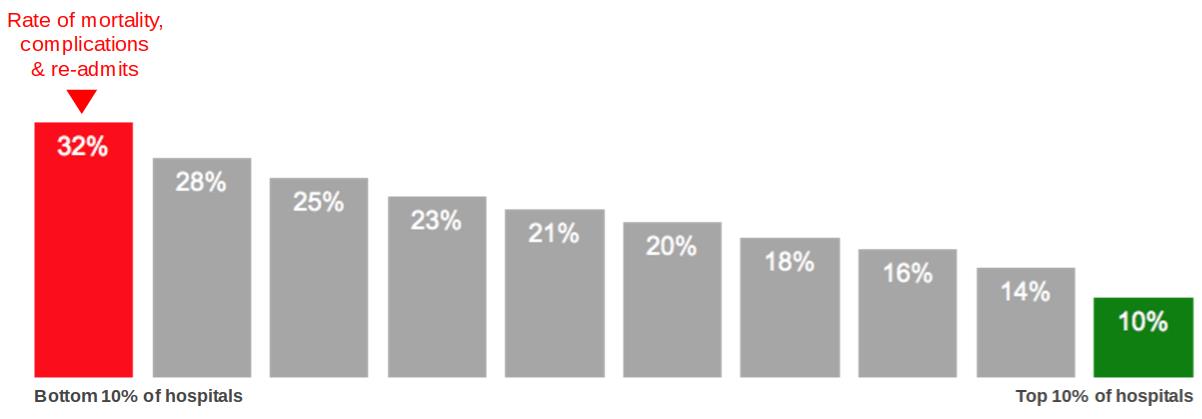
Figure 1: There is three times higher risk for adverseoutcomes at the worst performing hospitals (red) compared to thebest performing hospital (green) for gallbladder surgery.Source: Annals ofSurgery.
|Complications lead to extended hospital stays and readmissions,and ultimately translate to higher costs and more suffering forpatients. In a 2011 study published in the Annals of Surgery, theinvestigators found that a procedure resulting in severecomplications costs nearly six times more than the same procedurewith no complications.
|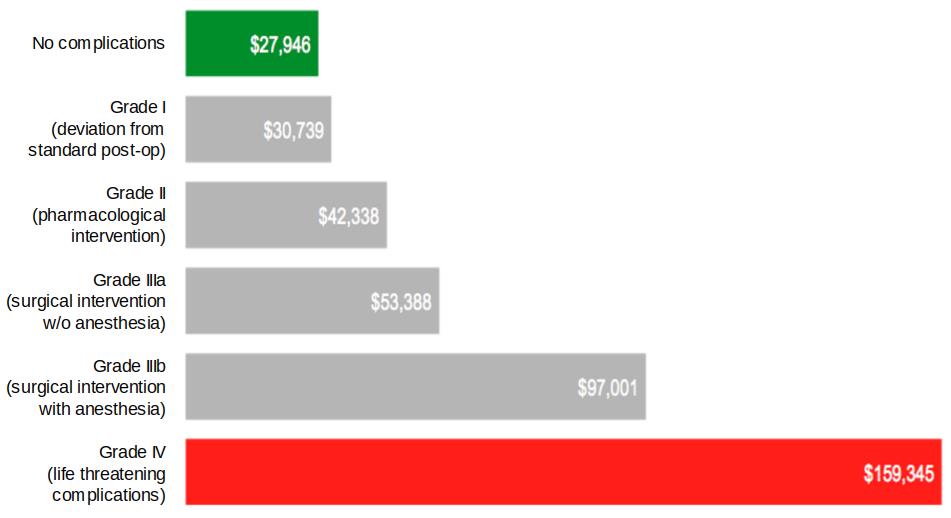
Figure 2: A procedure with severe complications costs almost6x more than the same procedure with no complications. Source:Annals ofSurgery.
|That well-negotiated $18,000 sticker price on knee surgery,which saved a self-insured employer $10,000 upfront, has thepotential of quickly turning into $100,000 if a major complicationoccurs, and this does not take into account the indirect costs oflost productivity, not to mention unnecessary patient suffering.
|The search for quality
It’s clear that the term "center of excellence" needs to beredefined. Here are the five critical steps to truly achieveexcellence.
|1. Ruthlessly ignore reputation
|The first step in selecting better centers of excellence is toput your preconceptions aside and become reputation agnostic. Asnoted, reputation does not always correlate to quality. Case inpoint: A Chicago hospital, touted as a “nationally recognizedleader” according to their website, was recently selected by a verylarge self-insured employer as a center of excellence for knee andhip surgery. The hospital’s orthopedic department is considered “#1in all parts of Chicago,” which is presumably what helped thembecome a center of excellence to great fanfare.
|Unfortunately, three continuous years of outcomes data does notsupport the hospital’s reputation. When examining risk-adjustedsevere complications and overall adverse outcomes, the abovereferenced hospital ranks far below the national average ofperformance for orthopedics providers in the country. When it comesto knee and hip replacement surgery, it performed at the absolutebottom. In terms of long-term clinical outcomes for theseprocedures, on a 100 to 800 point scale, their quality scores forboth procedures are at the poorest performance of 100. To furtherillustrate how reputation doesn’t matter, one of the best hospitalsin the country for knee replacement surgery is an all but unknownfacility — Valley Baptist in Harlingen, Texas. Yet, despite lackinga national brand name, Valley Baptist has performed at the absolutetop on the scale with a score of 800. As these examples show, oneshould heavily discount reputation as part of a center ofexcellence selection.
|2. Medical quality analytics: Don’t do ityourself
|Unless you’re a surgeon with a PhD in statistical analysis and adecade or two of experience grappling with medical performancedata, you need to find a team to perform the due diligencenecessary to evaluate whether a hospital is performing well. Withsome digging, an experienced health care analytics team would beable to direct a self-insured employer from the above mentionedreputable-but-poorly-performing Chicago hospital, to the equallyreputable but demonstrably high-performing Northwestern MedicineNetwork, including hospitals in the Greater Chicago area likeCentral Dupage in Winfield with a score of 710 in knee replacementsurgeryand Lake Forest Hospital with a score of 610 in hip replacement surgery.
|One of the biggest pitfalls we see with self-insured employersis the outsourcing of due diligence to organizations — includingemployer coalitions — lacking health care analytics or statisticscapabilities. If you wish to pursue the center of excellence model,it’s important to qualify the team and find people, organizationsor platforms that incorporate strong health care analyticsexperience.
|3. Outcomes, Outcomes, Outcomes
|The most important step in selecting true centers of excellenceis to focus on objective outcomes. Objective outcomes aremetrics that are measurable and not biased by perception. Forexample, mortality is an objective outcome. Complication rate is anobjective outcome. Readmission rate is an objective outcome. Bycontrast, patient satisfaction is not an objective outcome, because“satisfaction” is colored by things that do not meaningfullycontribute to health care results. In fact, there has been evidencethat shows that subjective outcomes like patient satisfaction areinverselycorrelated with effective patient care.
|With the 2013 and 2014 releases of massive Medicare providerdata, there is at least one publicly available data set for lookingat outcomes, and there are now a handful of analytics effortsranking and scoring the various hospitals based on these raw datasources. Importantly, when you look at health care quality metrics,make sure that whatever platform or methodology you choose, thereis risk adjustment for the patient population (meaning, hospitalswith sicker patients are not penalized for taking on thosepatients). Also, you must scrub the raw data and normalize itagainst facility variations, and you must have robust statisticalweighting to ensure a truly comparable rating system.
|4. Look for cost effectiveness
|You can stop at step three if you like, because outcomes-basedquality is the minimum standard for selecting a center ofexcellence. However, for most self-insured companies, loweringhealth care cost is a major motivator. To this end, a filter basedon cost can be applied to find the best providers with the lowestcost as a final step. You can take your list of excellent providersand your table of costs for each procedure and map them to oneanother.
|Now, if you think low cost and high quality are mutuallyexclusive, think again. As noted earlier, lower quality actuallycosts more money because of longer hospital stays and more medicalintervention. While health care costs can be complex, just lookingat the orthopedics price data from North Texas as reported in the Dallas Morning News,combined with knee replacement quality scores, you can see that thelowest cost hospitals are amongst the highest quality providers inthe group.
|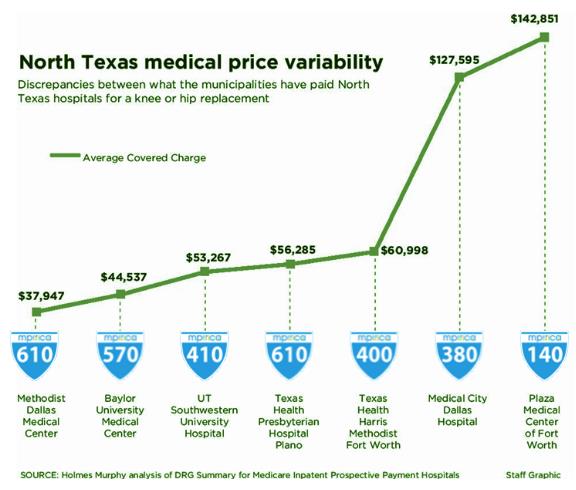
Figure 3: There is very little correlation between qualityof surgeries and the price to self-insured employers. Sources:Dallas Morning Newsand MPIRICAHealth.
|5. Direct procurement
|Once you establish quality and find value, the final step is toengage with the hospital organization to establish a relationshipfor direct procurement of services. The core tenet of a center ofexcellence model is negotiating a relationship that is a win-winfor both the provider and self-insured employer. The key featuresof the relationship should include reference-based bundled price,fast cash payment and quality monitoring. These relationshipsencourage ongoing quality and efficiency from the hospital, andallows the employer to steer patients to the provider by offeringincentives like zero out-of-pocket costs or cash back.
|The take-home message
|Finding and contracting with a center of excellence for specificprocedures is a great way to lower costs for self-insuredemployers, but it takes a bit of legwork. However, if you followthe steps laid out above, you will be able to take advantage of theCOE trend, save money, and protect your most important asset: youremployees. This is what a true win for everyone lookslike.
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Critical BenefitsPRO information including cutting edge post-reform success strategies, access to educational webcasts and videos, resources from industry leaders, and informative Newsletters.
- Exclusive discounts on ALM, BenefitsPRO magazine and BenefitsPRO.com events
- Access to other award-winning ALM websites including ThinkAdvisor.com and Law.com
Already have an account? Sign In
© 2024 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.