Workers who engage in health-smart habits offered in consumer-driven health plans reduced their health risks and lower their total medical costs an average of $9,700 per employee over a five-year period, according to a study of health care claims representing 1.1 million Cigna customers in CDHPs, PPOs and HMOs.
| The sixth annual Cigna Choice Fund Experience Study, released Wednesday, shows individuals enrolled in Cigna Choice Fund, Cigna's consumer-driven health plan, lowered their costs "without compromising care by becoming more engaged, informed and active health care consumers."
The sixth annual Cigna Choice Fund Experience Study, released Wednesday, shows individuals enrolled in Cigna Choice Fund, Cigna's consumer-driven health plan, lowered their costs "without compromising care by becoming more engaged, informed and active health care consumers."
Cigna's CDHP pairs a qualified medical plan with a health savings account or health reimbursement account. According to the study, when compared to customers in traditional PPO and HMO plans, those in a CDHP:
|- Lowered their health risks. CDHP customers lower their risk of developing or worsening a chronic condition. According to the study, when employers fully transitioned to offering only a CDHP option, individuals improved their health risk profile by 10 percent in the first year compared to customers in a traditional plan option.
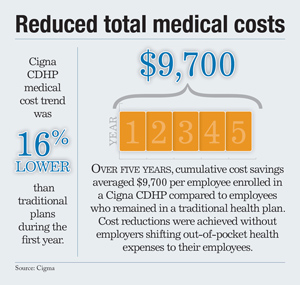
- Reduced total medical costs. Cigna CDHP medical cost trend was 16 percent lower than traditional plans during the first year. Over five years, cumulative cost savings averaged $9,700 per employee enrolled in a Cigna CDHP compared to employees who remained in a traditional health plan. Cost reductions were achieved without employers shifting out-of-pocket health expenses to their employees.
- Received higher levels of care. Cigna CDHP customers had consistent or higher use of over 400 evidenced-based medical best practices (than their counterparts in traditional plans). Those CDHP patients also sought preventive care—such as annual office visits and mammograms—more frequently than customers enrolled in a traditional plan.
- Were more engaged in health improvement. Through proper plan design plan and the use of incentives, CDHP customers were more likely to have completed a health risk assessment and participated in the Cigna Health Advisor health coaching program than those enrolled in a traditional plan.
- Were more savvy consumers of health care. CDHP customers enrolled in Cigna Pharmacy Management were more likely to choose generic medications and had 14 percent lower pharmacy costs compared to those in a traditional plan. Additionally, CDHP customers used the emergency room at a 13 percent lower rate than individuals enrolled in HMO and PPO plans.
- More likely to compare cost and quality. CDHP customers were twice as likely to use myCigna.com online cost and quality information to help them select a doctor or to review potential medical costs than customers enrolled in traditional plans.
"Each year the evidence increasingly shows that properly designed consumer-driven health plans can lower health risks, reduce medical costs and drive engagement," says Cigna Chief Medical Officer, Dr. Alan Muney. "The data once again shows that the combination of incentives, easy-to-engage health programs, and consumer decision support tools can improve health while reducing costs."
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Critical BenefitsPRO information including cutting edge post-reform success strategies, access to educational webcasts and videos, resources from industry leaders, and informative Newsletters.
- Exclusive discounts on ALM, BenefitsPRO magazine and BenefitsPRO.com events
- Access to other award-winning ALM websites including ThinkAdvisor.com and Law.com
Already have an account? Sign In
© 2024 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.








