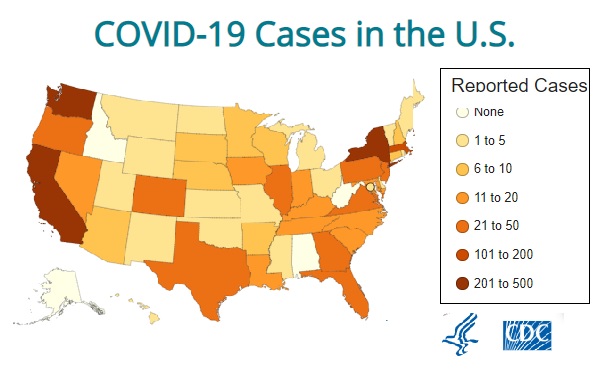
 (Credit: CDC)
(Credit: CDC)
The Centers for Medicare and Medicaid Services (CMS) has announced that the diagnosis and treatment of COVID-19 pneumonia are part of the "essential health benefits" package.
That means that, under federal rules, every individual or small-group major medical insurance policy that meets the Affordable Care Act (ACA) benefits standards should provide at least as much coverage for COVID-19 care as for care for ordinary strep throat, or a broken leg.
Related: Health insurers to waive cost-sharing requirements in fight against COVID-19 coronavirus
The Centers for Disease Control and Prevention has issued guidelines that recommend
But the essential health benefits package coverage rules don't apply to self-funded employer health plans. Self-funded fall under the jurisdiction of the U.S. Department of Labor's Employee Benefits Security Administration, and they do not have to meet the ACA essential health benefits coverage standards.
Even if a plan does have to meet the ACA essential health benefits coverage standards, the CMS guidelines don't directly affect what that plan does about co-payments, deductibles or other cost-sharing requirements.
The CMS guidelines also have no effect on "grandfathered" plans, or coverage that has been in place, with minimal changes, since before all ACA benefits standards took effect.
State insurance regulators are in charge of the benefits standards for fully insured health insurance policies, including grandfathered major medical policies, Medicare supplement insurance policies, and "non-ACA" health insurance policies, such as short-term health insurance policies.
Most states have been arranging for state-regulated health insurers to:
- Cover testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19 pneumonia, without imposing cost-sharing requirements on the patients, either through formal regulatory actions or through informal agreements with the health insurers.
- Ease preauthorization requirements related to COVID-19 testing.
- Cover or expand coverage of telehealth services.
- Provide an in-network level of coverage for patients who seek out-of-network care due to COVID-19-related health care system disruption.
- Cover early refills of enrollees' prescription medications, to help enrollees prepare for quarantines or other events that might make it difficult for the enrollees to get to drug stores.
- Cover any COVID-19 vaccine that becomes available with no cost-sharing.
Each state is presenting SARS-CoV-2 benefits guidelines and other SARS-CoV-2 coverage guidelines in its own way.
Here's a guide to all of the state SARS-CoV-2 health insurance rules and guidelines sites we could find, along with notes about efforts that go beyond the standard emergency response guidelines.
Alabama
Alaska
- Alaska Covid-19 announcements. (In the Headlines section, on the home page.)
- The bulletin for insurers.
Arizona
Arkansas
The Arkansas Insurance Department has not posted formal guidance, but Arkansas BlueCross BlueShield provides coverage for the majority of Arkansas residents.
California
Colorado
Connecticut
Delaware
District of Columbia
DC Health Link has developed a spreadsheet that shows how all district-regulated health insurers are covering Covid-19 care.
As of March 12, all issuers were covering testing without cost-sharing, and all classified Covid-19 treatment as a covered benefit.
Florida
- The Florid Covid-19 information page.
- The cost-sharing bulletin for health insurers.
- The prescription refill bulletin for health insurers.
Insurance regulators in Florida, as in a few other states, have published formal business continuity guidelines for insurers. The Florida bulletin gives insurers advice about what to do if, due to Covid-19, their "business operations are compromised to the extent that it jeopardizes the company's ability to provide essential insurance services."
Georgia
- Links to Covid-19 documents are available under the Insurance News and Directives tabs here.
- A Covid-19 preparedness and cost-sharing directive for health insurers.
- A directive that discourages Covid-19 testing labs from price gouging and waives in-person agent continuing education requirements through April 30.
Hawaii
Idaho
- The Idaho Covid-19 resources page.
- An announcement about Idaho health insurers' voluntary decision to waive Covid-19 test cost-sharing.
Illinois
- The Illinois Covid-19 benefits guide for consumers.
- The bulletin for health insurers and travel insurance providers.
The bulletin states the following about travel insurance:
Unless a travel insurance policy contains an exception applicable to Covid-19, a policy of travel insurance that covers the risks of sickness, accident, or death incident to travel presumptively must cover such risks relating to Covid-19. The extent of coverage for health care services, including emergency transportation within a foreign country, as well as the costs of returning to the United States for further treatment, may depend on the terms and conditions of the policy.
Indiana
The Indiana Department of Insurance has posted a guide to how 14 insurers in the state are handling Covid-19 testing on its home page.
All insurers contacted said they are covering Covid-19 diagnostic testing cost-sharing waived. Some are covering testing without cost-sharing only at approved locations.
Iowa
The Iowa Insurance Division says on the resources page that the four big major medical insurance issuers in Iowa and the Iowa Farm Bureau Health Plan have all agreed to waive cost-sharing for Covid-19 testing.
Kansas
Kentucky
- Kentucky Covid-19 insurance announcements. (In the Announcements section, on the home page)
- The state of emergency executive order.
Louisiana
Maine
- The Maine Bureau of Insurance Covid-19 insurance information page.
- An emergency measures bulletin for health insurers.
Maryland
- The Maryland Covid-19 information page.
- A collection of Covid-19 bulletins for health insurers is available here, in the 2020 section.
- A set of answers to questions about Covid-19, which includes discussions about interactions with life insurance and disability insurance.
Massachusetts
- The Massachusetts Covid-19 guidance page.
- The bulletin for health insurers.
- A bulletin announcing a special enrollment period for major medical insurance that will last until April 25.
Michigan
- Michigan coronavirus news.
- An announcement that "a number of insurers" have announced that they will cover medically necessary Covid-19 testing without cost-sharing.
Minnesota
Mississippi
Missouri
Montana
Nebraska
- A discussion of Nebraska health insurers' voluntary decision to waive Covid-19 testing cost-sharing.
Nevada
New Hampshire
New Jersey
New Mexico
- The New Mexico Covid-19 information page.
- The bulletin for health insurers.
- An order requiring benefits of health insurance products other than major medical insurance policies to notify the insureds that the policies may not protect them against Covid-19 expenses.
New York
North Carolina
- The North Carolina bulletins feed.
- The cost-sharing bulletin for health insurers.
- The prescription refill bulletin.
North Dakota
- The North Dakota Covid-19 bulletin announcement.
- The bulletin for health insurers and travel insurers.
The travel insurance provision states:
Unless a travel insurance policy contains an exception applicable to Covid-19, a policy of travel insurance that covers the risks of sickness, accident, or death incident to travel presumptively must cover such risks relating to Covid-19. The extent of coverage for health care services, emergency transportation within a foreign country, as well as the costs of returning to the United States for further treatment [may depend on the terms and conditions of the policy].
Ohio
The travel insurance provision states:
Issuers of travel insurance are reminded that unless a specific exclusion applicable to Covid-19 applies, a travel insurance policy that covers sickness, accident, disability, or death occurring during travel must cover such risks related to Covid-19 according to the terms of the policy. Many travel insurance policies also must cover cancellation or interruption of a trip or event, emergency transportation and/or costs of returning to the United States for further treatment pursuant to the terms of the policy.
Oklahoma
Oregon
Pennsylvania
Rhode Island
- The Rhode Island Covid-19 information page.
- Information about a special enrollment period for major medical insurance that will be available until April 15.
South Carolina
South Dakota
Tennessee
- The Tennessee Department of Commerce & Insurance Covid-19 guidance page.
- A bulletin for health insurers.
Texas
Utah
Vermont
Virginia
Washington
Washington state's order applies to issuers of short-term health insurance as well as to major medical insurance issuers.
West Virginia
- The West Virginia bulletins and orders. (In the Headlines and Events section.)
- A bulletin for health insurers.
- A business continuity bulletin.