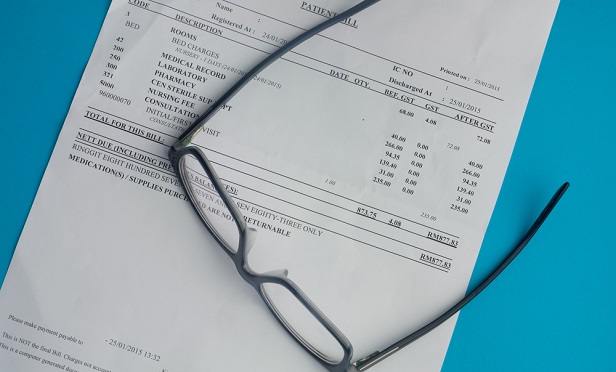
 Yes, while out-of-network bills are an unpleasant reality for too many Americans, there is some justification for them. (Photo: Shutterstock)
Yes, while out-of-network bills are an unpleasant reality for too many Americans, there is some justification for them. (Photo: Shutterstock)
When the Senate announced last week a bipartisan bill to put an end to surprise medical bills, it seemed like a slam dunk: finally, something Democrats and Republicans could agree on! Who wouldn't want to put an end to costly, often unexpected out-of-network medical bills burdening health care consumers?
Out-of-network providers who don't want to be beholden to price constraints set by outsiders, that's who.
In response to the Senate proposal, the Association of American Physicians and Surgeons issued a statement shedding light on the other side of the debate: the harm done to independent providers. Such regulations would give too much power to managed-care organizations, AAPS argues, allowing “third-party payers that are effectively accountable to no one” to set prices, which will drive out independent providers who do not participate in a carrier's network.
Continue Reading for Free
Register and gain access to:
- Breaking benefits news and analysis, on-site and via our newsletters and custom alerts
- Educational webcasts, white papers, and ebooks from industry thought leaders
- Critical converage of the property casualty insurance and financial advisory markets on our other ALM sites, PropertyCasualty360 and ThinkAdvisor
Already have an account? Sign In Now
© 2024 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.








